Azoospermia
Dr. Chaabane works with a team of gynecologists, geneticists and biologists specializing in
the management of hypofertile couples.

Azoospermia is defined as a male fertility disorder in which no sperm are present during ejaculation. This represents a percentage of 1% of the male population globally.
Male infertility is present in 50% of couples who have problems at the time of conception, since in 30% of the cases the origin of the problems is only of the man and in 20% of the cases, the infertility is due to a mixed cause, both sexes being equally involved. Among men suffering from male infertility, azoospermia occurs in a proportion that varies from 10% to 15% of cases.
There are two types of azoospermia depending on the origin of the lack of sperm in the semen:
- Secretory azoospermia (also called non-obstructive azoospermia): The problem is that the testes are not able to produce sperm.
- Excretory azoospermia (also called obstructive azoospermia): the testes synthesize sperm but there is a problem in the vas deferens which are responsible for transporting them to the urethra where they are expelled during ejaculation.

To diagnose azoospermia, according to WHO recommendations, it is necessary to perform two spermograms, at least two months apart, to confirm the results.
The search for the cause involves bacteriological, hormonal, genetic analyzes and sometimes imaging.
Obtaining a natural pregnancy with azoospermia is practically impossible. Procreation treatments will have to be used. However, depending on the type of azoospermia, the chances of becoming biological fathers vary. In the case of obstructive or excretory (non-secretory) azoospermia, there is a 100% chance of becoming a biological father. But in the case of secretory azoospermia, the probability decreases to 50%, if there are no other fertility problems.
Testicular Sperm extraction (TESE)
It is an outpatient surgical procedure that lasts 20 minutes and is performed under local or epidural anesthesia. It involves making a small incision to extract internal fragments of the testis that will be analyzed to detect the presence or absence of sperm.
Often, the semen obtained from the testicular biopsy is frozen for later use in fertility treatment (IVF).
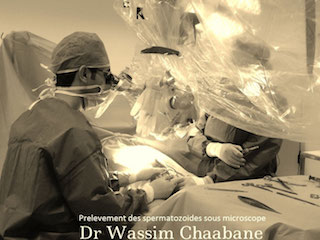
Micro-TESE

For patients with poor prognosis (small testicular size, hormonal abnormalities, history of testicular ectopia, genetic disease, etc.) or also in patients who have had a negative conventional testicular biopsy, foci of isolated spermatogenesis where we could isolate a few spermatozoa (nearly 20%) !! These sperm can be used fresh or frozen for ICSI.
The biopsy is then done under a microscope (micro-TESE). It is performed under loco-regional or general anesthesia and it can last between 2 and 5 hours. This technique is practiced in a few assisted reproduction centers around the world, including ours.
Cabinet d'urologie
Dr Wassim Chaabane
Centre Médical Coral
Centre Urbain Nord, 1082 Tunis
كورال الطبي
المركز العمراني الشمالي تونس
+216 71 947 574
Traitements innovants
Enucleation Prostatique au plasma
Laser pour calcul
micro-TESE
Varicocèle
Contact
Téléconsultation
A Propos